Discover the causes and effective solutions for psychophysiological insomnia. Learn how to break the cycle of sleep disorders with proven treatments like CBT-I.
Table of Contents
Understanding Psychophysiological Insomnia: Causes and Solutions
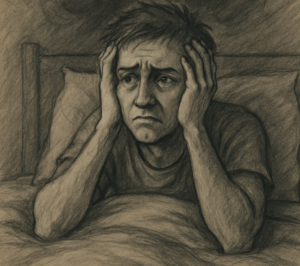
It’s 2 AM. You’re bone-tired, but your mind is running a marathon. You glance at the clock and start the familiar, painful math: “If I fall asleep now, I can still get four hours.” An hour later, you’re still wide awake, and a wave of anxiety washes over you. If this nightly dread sounds familiar, you are not alone, and there is a concrete reason your bed has stopped feeling like a sanctuary.
This frustrating experience is one of life’s cruelest paradoxes: the more desperately you try to sleep, the more it slips through your fingers. This isn’t a personal failing or a lack of willpower. In fact, for many people, the very effort to control sleep is what pushes it away. Sleep is a process of surrender, not of achievement, and trying to force it only activates the alert, problem-solving part of your brain that needs to be quiet.
Over time, this struggle creates a powerful and negative association. Your brain begins to learn that the bedroom is a place of frustration and anxiety. Your bed, once a place of rest, transforms into a stage for what feels like a nightly performance—and with it comes a heavy dose of what experts call sleep performance anxiety. This explains why you get anxiety before bed; your mind and body are simply preparing for the struggle they’ve come to expect.
Breaking this cycle begins with understanding it. This pattern of learned sleeplessness has a name, and because it is a learned response, it can also be unlearned. The goal isn’t to find a magic trick for how to stop worrying about not sleeping, but to gently retrain your brain to see your bed as a place of peace again.
The Snowball Effect: How a Few Bad Nights Become a Chronic Problem
It often starts with something ordinary. A stressful project at work, a sick child, or even just a few nights of excitement over an upcoming trip. For a short time, your sleep is disrupted, which is perfectly normal. But then, something subtle shifts. You stop worrying about the original trigger and start worrying about sleep itself.
Suddenly, the problem isn’t the looming deadline anymore; it’s the fear of another night spent staring at the ceiling. This is the critical turning point where temporary sleeplessness can transform into a chronic, looping pattern. The anxiety you feel about not sleeping becomes the very thing that keeps you awake.
This self-fulfilling prophecy creates a vicious cycle that can feel impossible to escape. For most people, the pattern of this mind-body connection looks something like this:
- The Trigger: A period of stress or illness causes a few nights of poor sleep.
- The Worry: You begin to dread bedtime, anticipating a struggle and worrying about how you’ll function tomorrow.
- The Arousal: This worry puts your mind and body on high alert, as if you’re preparing for a threat. Your heart might beat a little faster, and your thoughts start to race.
- The Result: This state of high alert is the opposite of the calm needed for sleep. You lie awake, which confirms your fear and strengthens the cycle for the next night.
Over time, your brain becomes incredibly good at running this program. It learns to associate your entire bedtime routine with anxiety instead of rest. Soon, the problem isn’t just in your head; it feels like your own bedroom has turned against you.
“My Bed Is the Enemy”: Understanding Conditioned Arousal
Have you ever found yourself nodding off on the couch, only to become instantly wide awake the moment you get into bed? This isn’t a coincidence; it’s a classic sign of what experts call conditioned arousal. Over time, your brain has learned a powerful, unconscious lesson: the couch is for relaxing, but the bed is for the stressful work of trying to sleep. This is the heart of what is known as conditioned or learned insomnia.
Think of it like getting a mild case of food poisoning after eating at a specific restaurant. Months later, just driving past that restaurant might make your stomach turn, even though you’re perfectly healthy. Your brain created a negative association. In the same way, after weeks of tossing and turning, your brain has started to associate your bedroom not with rest, but with frustration and anxiety. The moment you walk into the room, your body automatically prepares for a struggle, releasing stress hormones that make sleep feel impossible.
The battle for sleep isn’t won by trying harder. You can’t force yourself to relax any more than you can force yourself to like a food that once made you sick. The real goal is to break this negative connection and retrain your brain to see your bed as a safe, peaceful sanctuary once again. To do that, we must first understand why your brain’s internal alarm system became so sensitive in the first place.

Why Your Brain’s “Smoke Detector” Is Too Sensitive
That internal alarm system we mentioned? Think of it like a smoke detector that has become overly sensitive. It’s supposed to go off for a real fire, but instead, it’s being triggered by the tiniest puff of smoke—like the mere thought of not sleeping. This constant state of high alert has a name: hyperarousal. It’s not just a feeling of being worried; it’s a full-body physical state where your nervous system is braced for danger, even when you’re safe in bed. This is the root of the mind-body connection and sleep problems that so many people face.
This state of hyperarousal is essentially your body’s “fight-or-flight” response being activated at the worst possible time. When your brain anticipates a struggle in the bedroom, it floods your system with stress hormones like adrenaline and cortisol. These are “wake-up” chemicals designed to make you sharp and ready for action, not calm and ready for sleep. This is why you can feel utterly exhausted mentally but physically feel “wired,” with a racing heart, tense muscles, and a mind that just won’t quit.
In this revved-up condition, sleep isn’t a choice. It’s chemically and physically out of reach. You can’t simply will your body to shut down when it’s been told to prepare for a threat. This understanding is crucial: you aren’t failing; your body is just following a faulty command. This entire cycle—a worried mind triggering a hyperaroused body—has a specific name, and defining it is the first step toward a real solution.
Putting a Name to the Problem: What Is Psychophysiological Insomnia?
This entire pattern—the worried mind triggering a hyperaroused body—is a well-understood condition with a formal name: psychophysiological insomnia. While the term sounds clinical, the concept is simple. “Psycho” refers to your mind, including the thoughts and anxieties you have about sleep. “Physio” refers to your body and the physical state of high alert it enters. Put together, it describes a vicious cycle where your mind and body have learned to work against sleep.
Essentially, this is a form of chronic insomnia rooted in conditioned arousal. It explains why you might feel sleepy watching TV on the couch but become instantly wide awake the moment you get into bed. Your brain has formed a powerful association between your bedroom and the frustrating act of trying to sleep, rather than the peaceful act of resting. It’s not that you’ve forgotten how to sleep; it’s that your bed has accidentally become the trigger for wakefulness.
Giving this struggle a name is incredibly powerful. It shifts the problem from being a personal failing to a recognized medical pattern. You are not “bad at sleeping.” Instead, your body is running a faulty program that can be corrected. This distinction is crucial; knowing the specific nature of psychophysiological insomnia explains why generic advice often falls short.
“But I’ve Tried Everything!”: Why Basic Sleep Hygiene Fails for This Condition
If you’re dealing with psychophysiological insomnia, you’ve likely heard the term “sleep hygiene” more times than you can count. You’ve probably tried it all: the dark room, the consistent bedtime, the ban on late-night caffeine. The frustration when none of it works is immense, often leading to the feeling that you are somehow broken or failing at something that should be natural. But the problem isn’t your effort—it’s that you’ve been given the wrong tools for this specific job.
Think of standard sleep hygiene as general maintenance for a healthy sleep system. It’s excellent advice for someone whose sleep is occasionally disrupted by poor habits. However, it does nothing to address the core of psychophysiological insomnia: the learned anxiety and mental hyperarousal. Following these rules can’t fix a brain that has come to associate the bedroom with a state of high alert. It’s like tidying a house when the real problem is a faulty fire alarm that goes off every night—no amount of cleaning will stop the siren.
This is precisely why a more powerful approach is needed. You can’t simply will your brain to stop being anxious. Instead, the goal is to actively retrain the conditioned response your mind and body have developed around sleep. Breaking this cycle isn’t about adding more rules or trying harder; it’s about unlearning the fear and rewiring the connection between your bed and rest. This is not only possible, but it is the key to finding lasting relief.
The Path Forward: You Can Retrain Your Brain to Sleep
The most hopeful truth about a learned problem is that it can be unlearned. Your brain is not permanently wired for wakefulness; it is remarkably adaptable. Just as it created a negative association between your bed and anxiety, it has the capacity to forge a new, positive one. This process isn’t about wishing it away—it’s about actively guiding your brain back to a state where the bedroom once again signals safety and rest, not a nightly battle.
Overcoming the fear of sleeplessness means shifting your goal entirely. Instead of trying to force sleep, the objective is to teach your brain that the bedroom is no longer a threat. Think of it like reassuring a frightened animal; you don’t command it to calm down. You create a safe environment and, through consistent actions, show it there is nothing to fear. Over time, its nervous system learns to relax on its own. Your brain works in much the same way.
Fortunately, this retraining isn’t a matter of guesswork. It’s a science-backed journey using structured techniques designed specifically to dismantle the cycle of anxiety and teach your mind and body to let go of the hyperarousal that fuels insomnia. The most effective of these methods is known as Cognitive Behavioral Therapy for Insomnia, or CBT-I.
The Gold-Standard Treatment: An Introduction to CBT-I
So, what exactly is this treatment with the clinical-sounding name? Cognitive Behavioral Therapy for Insomnia (CBT-I) isn’t just another suggestion; it’s the single most effective, long-term solution for chronic insomnia. In fact, the American College of Physicians recommends it as the first-choice treatment—even before sleeping pills—because it equips you with lasting skills, rather than offering a temporary patch. It’s less like a medicine and more like a user’s manual for your own sleep system.
The “Cognitive” part of the therapy is all about your mindset. It’s a guided process for identifying and reframing the anxious thoughts that fuel sleeplessness, like “If I don’t sleep now, tomorrow will be a total disaster.” Instead of letting these catastrophic thoughts control your night, you learn practical ways to challenge their power, reducing the mental pressure and anxiety that keep your brain on high alert.
Meanwhile, the “Behavioral” component focuses on your actions and routines. For many with learned insomnia, the bed has accidentally become a stage for worry, not a sanctuary for rest. This part of the treatment uses simple, concrete strategies to systematically break that negative association. Through a few powerful changes in your habits, you effectively retrain your body to once again connect your bed with immediate, natural sleepiness.
Together, these two approaches dismantle the cycle of insomnia from both sides. This comprehensive cognitive behavioral therapy for insomnia guide gives you the tools to become your own sleep expert by targeting the root cause of the problem, starting with breaking the frustrating link between your bed and wakefulness.
CBT-I in Action (Part 1): Breaking the Bed-Anxiety Link with Stimulus Control
The first, most powerful step in this behavioral retraining is called Stimulus Control for Insomnia. Its goal is surgically precise: to break the connection your brain has made between your bed and a state of anxious wakefulness. To do this, you must teach your brain, through action, that your bed is only for sleep.
The rules are deceptively simple, but they work by systematically rewiring that learned association. This isn’t about punishment; it’s about protecting your sleep sanctuary.
- Use the bed only for sleep and intimacy. No more reading, watching TV, scrolling on your phone, or worrying in bed.
- If you can’t fall asleep (or fall back asleep) in about 20-30 minutes, get out of bed. Don’t lie there tossing and turning. The exact time isn’t what matters—the feeling of being frustrated and wide awake is your cue.
- Go to another room and do something quiet and boring. Read a dull book or fold laundry in low light. When you feel genuinely sleepy again, return to bed. Repeat as needed.
Getting out of a warm bed might feel like the last thing you want to do, but it is the most crucial step. Every minute you lie there stewing in frustration, you strengthen the mental link between “bed” and “anxiety.” By getting up, you stop feeding that negative connection. This is the core of learned insomnia treatment at home; you are actively taking control.
Over time, this practice retrains your mind. Your brain begins to understand that the bed is a place where sleep is expected to happen quickly and naturally. But changing your behavior is only half the equation. Next, we need to address the racing thoughts themselves.
CBT-I in Action (Part 2): Challenging Your Sleep-Stealing Thoughts
While Stimulus Control deals with your physical environment, what about the racing thoughts that can follow you right out of the bedroom? This is where the “cognitive” piece of CBT-I comes into play. The goal here is cognitive restructuring—a straightforward method for identifying, challenging, and changing the beliefs that fuel your insomnia. It’s about retraining your brain to stop treating sleeplessness like a catastrophe.
Much of this nighttime anxiety stems from a pattern called “catastrophic thinking,” where your mind takes a small worry and blows it up into a worst-case scenario. This creates intense sleep performance anxiety help. The first step is to recognize these thoughts aren’t facts, and then gently replace them with more balanced, realistic ones.
| Catastrophic Thought | Realistic Reframe | | :— | :— | | “If I don’t get 8 hours of sleep, tomorrow will be a total disaster.” | “I won’t feel my best, but I’ve managed on less sleep before. The day will be challenging, not a disaster.” |
This mental shift is one of the most powerful cognitive restructuring sleep techniques. By defusing these high-alert thoughts, you lower the emotional stakes and reduce the anxiety that keeps your body on guard. As you practice learning how to stop worrying about not sleeping, you can explore a final, surprising technique that flips the entire struggle for sleep on its head.
CBT-I in Action (Part 3): The Surprising Trick of Trying to Stay Awake
After spending so much energy challenging catastrophic thoughts, what if you could sidestep the battle for sleep entirely? This brings us to one of the most counterintuitive yet effective techniques in the CBT-I toolkit. It’s called paradoxical intention for sleep, and the instruction is simple: stop trying to fall asleep and, instead, gently try to stay awake. By giving up the struggle, you take away insomnia’s primary source of power.
This may sound absurd, but it’s a brilliant mental trick for providing sleep performance anxiety help. When you’re desperate for rest, your bed can feel like a stage where you must perform the act of sleeping. By deciding to stay awake, you’re essentially walking off that stage. Suddenly, there’s no goal to fail at. The pressure dissolves, which in turn reduces the hyperarousal that was keeping you vigilant and allows your body’s natural sleep drive to take over.
To practice this, simply lie in bed in the dark with your eyes open. Tell yourself you’ll just stay awake for a few more minutes. The real goal isn’t to force an all-nighter; it’s about overcoming fear of sleeplessness by proving to yourself that being awake in bed isn’t a threat. This mental technique for calming the mind works hand-in-hand with another powerful tool that physically retrains your body’s clock: creating a dedicated sleep window.
CBT-I in Action (Part 4): Consolidating Sleep with a Sleep Window
While paradoxical intention helps calm your mind, creating a “sleep window” retrains your body. If you spend eight hours in bed but only sleep for five, that’s three hours spent frustrated and reinforcing the idea that your bed is a place for wakefulness. The goal of this core technique in cognitive behavioral therapy for insomnia is to match your time in bed with the amount of sleep you’re actually getting, even if that means starting with just five or six hours.
Doing this accomplishes two critical things. First, it builds powerful sleep drive—your body’s natural hunger for sleep. Just as skipping lunch makes you ravenous for dinner, restricting your time in bed makes your body desperate for deep, consolidated rest. Second, it dramatically improves your sleep efficiency, which is simply the percentage of time you’re asleep in bed. A higher efficiency score retrains your brain to associate the bed with sleeping, not struggling.
This might sound like a form of sleep deprivation, but it’s actually the opposite. It’s sleep consolidation. Instead of getting fragmented, poor-quality sleep over a long period, you are aiming for a shorter but more solid block of rest. This is a temporary, therapeutic tool. The aim isn’t to live on less sleep forever; it’s to create a strong foundation of efficient sleep from which you can build.
As your sleep becomes more solid and your efficiency improves, your sleep window is gradually widened until you are getting the full amount of rest you need. This structured approach is a key part of any effective CBT-I guide because it physically breaks the cycle of learned insomnia. It’s about teaching your body to sleep well again, offering a lasting solution rather than a temporary patch. But how does this compare to simply taking a pill?
CBT-I vs. Sleeping Pills: A Long-Term Fix vs. a Short-Term Crutch
When you’re exhausted and desperate for rest, the promise of a sleeping pill can feel like a lifeline. It offers a simple, immediate answer to a complex problem. However, it’s crucial to understand the fundamental difference between borrowing sleep with medication and rebuilding your ability to sleep on your own. Pills work by inducing sedation—chemically pressing an “off” switch—while CBT-I works by addressing the root cause: the learned thoughts and behaviors that fuel the insomnia cycle.
Comparing the two approaches side-by-side makes the distinction clear when considering a chronic insomnia treatment:
- The Mechanism: Sleeping pills temporarily mask the symptom of sleeplessness. CBT-I provides skills to resolve the problem of sleep anxiety and hyperarousal.
- The Outcome: Medication offers short-term relief, but its effectiveness can wane, and it doesn’t prevent insomnia from returning. The skills from CBT-I are a form of learned insomnia treatment at home that you can use for the rest of your life.
- The Goal: The aim of a pill is to get you through the night. The aim of CBT-I is to give you back the confidence to sleep naturally, without needing any aid at all.
This difference is why the American College of Physicians recommends CBT-I vs sleeping pills as the first-line treatment for chronic insomnia. While medication can have a place in a crisis, it’s like using a crutch for a leg injury. The crutch helps you walk today, but physical therapy is what strengthens your leg so you can walk on your own tomorrow. CBT-I is the physical therapy for your sleep.
So, if this is the recommended path, how do you get started?
Finding Help: How to Access CBT-I Right Now
Fortunately, starting Cognitive Behavioral Therapy for Insomnia is more accessible than ever before. You don’t necessarily need a referral or a long wait to see a specialist. The right path for you depends on your budget, learning style, and desire for one-on-one support. The most important thing to know is that you can begin taking control of your sleep today.
There are three main pathways to get started, each offering a proven, structured approach to rebuilding your confidence in sleep:
- Digital CBT-I Programs: Evidence-based CBT-I apps like Somryst and Sleepio offer a complete, interactive cognitive behavioral therapy for insomnia guide right on your phone or computer. They are convenient, private, and allow you to begin immediately.
- A Trained Therapist: For personalized, one-on-one support, you can work with a psychologist or therapist trained in behavioral sleep medicine. The Society of Behavioral Sleep Medicine has an online directory to help you find a qualified provider in your area.
- Self-Help Workbooks: If you prefer to work at your own pace, a high-quality workbook can be an excellent form of learned insomnia treatment at home. Books like Say Good Night to Insomnia by Gregg D. Jacobs walk you through the very same techniques used in clinical settings.
Regardless of the path you choose, the goal remains the same: to systematically unlearn the anxiety and hyperarousal that have taken over your nights. By taking this first step, you are moving away from managing symptoms and toward a lasting solution.
Taking Back Your Nights: Your First Step to Breaking the Sleep Cycle
That feeling of being wide awake and frustrated, your bed a source of anxiety rather than comfort, is no longer a nameless struggle. You now see it for what it is: a predictable, learned pattern where your mind and body have gotten stuck in a state of high alert. The paradox of trying harder only to feel more awake finally makes sense.
For so long, the fight may have felt like it was against your own mind. But the real opponent was never your brain; it was the vicious cycle itself. This is the key to overcoming the fear of sleeplessness: realizing your insomnia is not a life sentence, but a habit your brain has learned. And what has been learned can be unlearned.
The first real step in how to break the sleep anxiety cycle is to seek out the tools designed to do the work for you, like Cognitive Behavioral Therapy for Insomnia (CBT-I). This is the proven way you can train your brain to sleep naturally again.
Your journey to better rest doesn’t begin when your head hits the pillow. It begins right now, with the empowering knowledge that you can stop fighting and start retraining. You are no longer just a person with insomnia; you are someone who understands it and holds the map to find your way back to rest.